In recent years, experts around the world have observed an increase in degenerative-dystrophic processes in the ankle, which has gradually led to disability. Anthrax of the ankle joint often develops due to severe injuries or permanent microtrauma in athletes, professional dancers, circus performers. In this article, you will learn how to detect signs of the disease in time and stop its progression, and how to treat it.
Ankle arthrosis - what is it
The ankle is a complex block-like joint formed by the lower (distal) ends of the tibia and fibula of the lower leg, forming the inner and outer ankles (ankles) and the tibia of the foot. It is reinforced on the inside by the deltoid ligament and on the outside by the anterior and posterior talofibular and calcaneofibular ligaments. Function: bend and stretch the foot. The ankle is functionally connected to the foot, with ligaments and muscles common to the joints of the foot.
Anthrax of the ankle joint is a degenerative-dystrophic disease that begins with the thinning and destruction of articular cartilage, reducing its damping properties and then involving all other joint tissues in the pathological process. The disease gradually leads to complete wear and disability of the joints. The ICD-10 code for ankle arthrosis is M19.
The disease is less common than a similar knee injury and is usually the result of serious injury or long-term injury from any activity.
Causes of ankle osteoarthritis
Specialists have studied in detail the causes of ankle arthrosis and leg arthrosis. This:
- injuries - intra-articular fractures of the joints, complete and incomplete rupture of the ankle fractures, ligaments and tendons;
- microtrauma due to any professional activity - these are ballerinas, dancers, professional athletes;
- increased load on the legs with excessive body weight;
- improper load distribution when wearing high heels;
- metabolic disorders that negatively affect cartilage metabolism - diabetes, obesity, gout, etc. ;
- hormonal, including age-related shifts;
- transmitted severe acute purulent arthritis;
- long-term chronic arthritis of any origin;
- osteochondrosis of the lumbar spine and an intervertebral hernia that causes damage to the roots of the spine and a weakening of the muscles of the leg and foot, leading to joint instability and injury.
Mechanism of disease development (pathogenesis)
For a variety of reasons, blood flow to the joint region causes a disorder that leads to a decrease in the volume of joint fluid that feeds cartilage tissue. Due to the lack of oxygen and nutrients, the cartilage becomes thinner and cracks and erosions appear on it. This leads to damage to the layer of bone below the cartilage. It thickens (sclerotizes) and grows along the edges of the joint surfaces. These increases are called osteophytes. They compress the soft tissues, blood vessels and nerves, causing pain and further disrupting blood circulation.
Due to circulatory disorders and high tension, the muscles suffer and weaken, which leads to joint instability and frequent displacement. Arthrosis of the foot develops, with the tarsus, metatarsal, metatarsal, and interphalangeal joints affected.
Gradually, connective tissue grows in the joints, tightly binding the joint surfaces and disrupting joint functions. Complete loss of ankle function results in fusion of the bone joints. Arthrosis of the foot also develops gradually.
Symptoms of ankle osteoarthritis
Ankle arthrosis first progresses slowly and unnoticed. But the symptoms gradually appear and worsen, indicating some violation of the lower limb.
First signs
The very first symptom of ankle arthrosis is pain during heavy exercise, such as long walks, dancing, soccer or volleyball, and so on. This pain goes away quickly, so one does not pay immediate attention to it, attributing it to muscle fatigue. Pain can be symmetrical in both joints (under heavy load and microtrauma) and unilateral (after major injury).
Then you feel stiff in the morning or after a long stay still. The ankles stiffen for a while, making it difficult to move. It lasts for a few minutes in the initial stage and goes away after slow pacing. This symptom should already be a warning and a reason to see a doctor.
Obvious symptoms
The post-exertional pain gradually intensifies and lasts longer. Your feet can hurt all day. Nocturnal pains join, usually occurring in the second half of the night and are sometimes accompanied by painful muscle cramps. Stiffness periods after immobility are also prolonged.
Due to the severe pain, the person starts limping while walking, trying to reduce the pain in the leg by stretching or pressing. Sometimes the ankle swells, the skin is red, and the pain increases. This is a sign of synovitis - inflammation of the inner joint membrane. Inflammation is non-infectious, develops as a result of mechanical irritation, and resolves on its own without treatment. However, exacerbation of synovitis activates the progression of the joint degenerative-dystrophic process.
Dangerous symptoms

Persistent aching pain exacerbated by physical exertion, instability, joint looseness, tendency to subluxation, dislocations, and ligament injuries are dangerous symptoms that require medical attention. The ankle changes externally: it takes on a different shape due to overgrown osteophytes. Ankle (ankle) leads to thickening of arthrosis. The movements of the foot are somewhat restricted at first, then the ankle becomes immobile or, conversely, loose, unstable. But even at this stage, the patient can only be helped by contacting the clinic. Symptoms of arthrosis of the foot appear: pain in the foot, violation of bending, and depreciation. The development of big toe arthrosis is accompanied by pain and deformity of the foot, in the form of bulge and buckling of the big toe.
What is dangerous ankle arthrosis
The danger is that the disease will go unnoticed at first, and very often the patient will seek medical attention at an advanced stage.
Any localization and form of arthrosis has serious complications, so you should not delay treatment.
Classification
Ankle arthrosis may be primary if the cause is unclear and secondary to known causes. Depending on the cause of the development, the disease may have its own characteristics.
Post-traumatic arthrosis of the ankle joint
The consequences of traumatic injury are the most common causes of the disease. Post-traumatic arthrosis of the ankle joint can develop after severe injury - ligament rupture, dislocation, intra-articular fracture. Usually a joint is damaged, so post-traumatic arthrosis is unilateral. A small but untreated injury may not make you feel at first. And only after a time when one has forgotten about it, a slightly increasing pain appears. This type of injury is dangerous because the patient already goes to the doctor in a neglected state. Severe injuries are treated better, the consequences appear faster, and the patient does not see a doctor until late.
Both ankles are inconspicuous, with long-term microtrauma characteristic of professional dancers, athletes, and people whose profession is related to long-leggedness. During exercise, there are symmetrical pains in the ankle. They are usually confused with muscle pain associated with fatigue, so it is also too late to see a doctor.
Ankle arthrosis after arthritis
These arthrosis can be caused by chronic inflammatory processes in the joints (arthritis): rheumatic, reactive, psoriatic. In this case, the inflammatory processes are combined with degenerative-dystrophic (arthritis-arthritis). This speeds up the process of ankle destruction. As the inflammation gets worse, the joints swell, the skin becomes red, and the pain becomes very severe, especially at night. When the inflammation subsides, metabolic disorders dominate while all processes progress very quickly. The disease requires constant monitoring and rheumatologist treatment.
More rarely, a degenerative-dystrophic process develops after acute purulent arthritis. The purulent process destroys the joint tissues, and after healing, connective tissue is formed, which disrupts the function of the limb.
Arthrosis can also develop after an infectious arthritis - tuberculosis, gonorrhea, etc. The progression of the disease is related to the main infectious process and the nature of the death. If the infection persists, the destruction of the joints progresses.
Metabolic
It develops with long-lasting gout. Very often the first toe is affected. Other small joints in the foot and ankle are less commonly affected. As gout attacks continue, it is difficult to determine externally when the degenerative-dystrophic process occurs. It can only be seen on an X-ray. In any case, the patient should be monitored regularly by a rheumatologist and examined periodically.
Deforming arthrosis of the ankle joint
All types of arthrosis deform over time. Bone deformities indicate an advanced stage of the disease, when the cartilage has already collapsed, and a constant mechanical impact on the bone tissue contributes to its growth along the edges of the joint surface. This is how osteophytes are formed, which change the shape of the joint.

Degrees of ankle arthrosis
There are several classifications, one of which distinguishes three clinical and radiological stages of arthrosis:
- Early. Slight pain after long standing or walking, some stiffness in the morning. All of this disappears quickly without help. X-ray: Normal or mild narrowing of the joint gap.
- advanced. The pain after physical exertion is stronger and longer. Stiffness increases, cracks appear in the joints during movement. Sometimes the joint swells, blushes and hurts a lot - this is a sign of synovitis. The radiograph shows a significant narrowing of the joint gap, thickening of the bone tissue under the cartilage (osteosclerosis) and proliferation of osteophytes.
- Final. The pain syndrome intensifies and becomes permanent. Because of the pain, a person limps, pulls his leg, uses a stick, or uses crutches. The function of the limb is impaired, and arthrosis of the foot and thumb develops. Complete absence of flexor-extensor movements is rare, usually in the background of arthrosis-arthritis. On X-ray: no joint gap, osteosclerosis, large osteophytes deform the joint.
Possible complications
If the disease is not treated and everything is allowed to go its own way, the following complications are possible:
- permanent joint dysfunction and disability;
- severe incessant pain in the ankle and foot, with or without exertion;
- ankle instability with the development of normal dislocations and subluxations;
- damage to the foot and thumb unites, further worsening the patient’s condition.
Diagnosis of ankle arthrosis
Before prescribing treatment, the doctor will examine the patient, including:
- medical interview and examination;
- additional research methods: laboratory examinations (detection of signs of inflammation and metabolic disorders), instrumental examinations (joint X-ray imaging, computer and magnetic resonance imaging - detection of early changes in bone structures and soft tissues), diagnostic arthroscopy (internal arthroscopy).
Treatment of ankle arthrosis
After making the final diagnosis, the doctor selects an individual treatment complex for the patient, consisting of pharmacological and non-pharmacological methods.
Medical treatment of ankle arthrosis
Medicines that are symptomatic (eliminate the symptoms of the disease) and pathogenetic (suppress the mechanism of the disease) are prescribed.
Anti-inflammatory and analgesic
To relieve pain, medicines in the group of non-steroidal anti-inflammatory drugs (NSAIDs) are prescribed in short courses that relieve pain and inflammation well (if the synovitis has got worse):
- injection;
- rectal suppositories;
- Oral tablets;
- skin patch.
Muscle relaxants
The muscles surrounding the patient’s joint that are moving are in constant tension, leading to atrophy and increased pain. Medications belonging to the group of muscle relaxants are prescribed to eliminate muscle cramps.
Chondroprotectors
Drugs belonging to the group of chondroprotectors contain glucosamine or chondroitin, and sometimes both. They protect cartilage cells from destruction and help restore them. They are prescribed in the form of injections, tablets and external agents (creams and ointments).
Hyaluronic acid preparations for ankle arthrosis
Hyaluronic acid is injected into the joint cavity to improve the cushioning ability of the synovial fluid and to prevent further damage to cartilage and bone tissue. This results in pain relief and better joint mobility.
Gels and ointments for arthrosis of the ankle joint
External devices can also be used at home. Ointments for ankle arthrosis:
- NSAID gels are suitable for relieving pain and inflammation;
- cartilage recovery - chondroitin-based gel and ointment.
Non-drug therapy
The main methods of treating ankle arthrosis are non-pharmacological. These are therapeutic exercises, massage, physiotherapy, wearing orthopedic devices.
Physiotherapy
The following should be prescribed to alleviate the patient's condition and restore joint function:
- electrophoresis with medicinal substances;
- laser therapy;
- magnetotherapy;
- use of sludge for heating processes - paraffin, ozocerite, resort conditions.
Massage for arthrosis of the ankle joint
Massage treatments improve blood circulation, which leads to the activation of metabolism and the restoration of joint and extraarticular tissues. The positive effect of massage on the muscles is the elimination of the spasm, which contributes to the blood flow to the muscles and the restoration of the strength needed to keep the limb in the desired position.
Exercises and gymnastics for ankle arthrosis
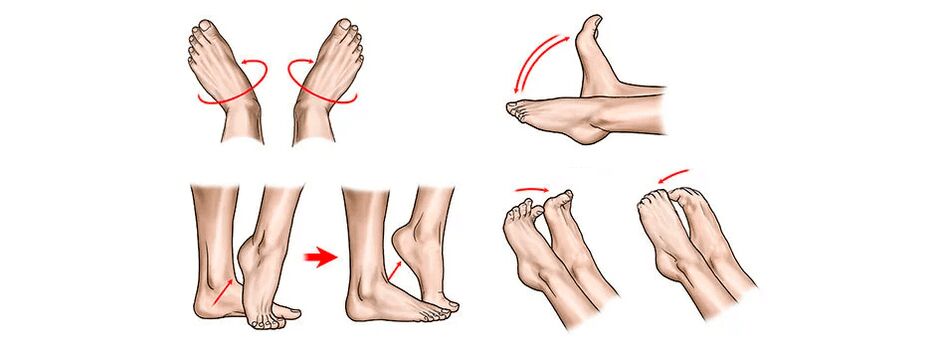
Physiotherapy is a panacea for arthrosis. Motor activity is very important, swimming is useful in addition to movement therapy. Systematic implementation of exercises selected by the physician will allow the limb to be largely restored to function, even in advanced disease.
An approximate set of exercises (but consult your doctor before starting the exercise):
Use of special orthopedic products
To prevent the disease from progressing, your doctor may require you to wear a special orthopedic device called an orthosis. It fixes the foot in the proper anatomical position, relieves muscle tension, improves blood circulation. The doctor will prescribe the orthosis to wear and will also select the most appropriate model.
The ankle can also be fixed with tape: special adhesive tapes are used to gently secure the ankle in the desired position.

Surgical intervention
Surgery is recommended for severe pain that is not treated with conservative treatments and for significant limb dysfunction.
Types of surgical procedures
The operations can be performed in traditional and gentle ways:
- Therapeutic arthroscopy (gentle surgeries):
- joint cavity hygiene - arthroscopy removes fragments of cartilage and bone tissue from the cavity that interfere with movement and cause pain;
- cartilage - the damaged layer of cartilage is removed, which stimulates the growth of new cartilage cells (abrasive cartilage); in some cases, transplants (mosaic arthroplasty) are taken from autoporous sections taken from the unloaded areas of the patient's knee joint; Chondroplasty is effective in stage 2 of the disease when the joint has not yet lost its function.
- Arthrodesis is a traditional surgical operation. It is performed with significant violation of limb function, looseness, normal dislocations, and pain. The joint is removed, the bones of the leg are joined to the bones of the foot. The ankle becomes immobile and only serves as a support.
- An endoprosthesis is the replacement of a worn and lost ankle function with an artificial one.
Characteristics of postoperative rehabilitation
All operations are performed under stationary conditions and then experts recommend full rehabilitation. With gentle surgeries, rehabilitation is performed on an outpatient basis, with early integration into therapeutic practices, except for high loads on the joints. After the endoprosthesis, the patient stays in the hospital for a week and then undergoes outpatient rehabilitation measures. After two weeks, the sutures are removed and the patient can take a shower.
Dietary foods
There is no special diet for osteoarthritis. But to eliminate unnecessary stress on the ankle, you need to maintain a normal body weight. One should get a proper healthy diet, but the amount of high calorie foods should be partially replaced by vegetables and fruits. Low-fat first and second courses, chicken, sea fish, cottage cheese, cheese, dairy products are useful.
Traditional medicine
Traditional medicine alone does not help treat arthrosis. But they can be used as part of a complex treatment prescribed by a doctor. Here are some recipes:
- for oral administration: infusion of wild rosemary; Pour 20 g of finely chopped herbs into a thermos overnight with 500 ml of boiling water, strain in the morning and take with half a glass four times a day for a month; analgesic, restores cartilage tissue;
- for oral administration: take a 0. 5 cm diameter mummy ball in the morning, chewing thoroughly, 30 minutes before a meal for 10 days; Pause for 5 days, then repeat everything 3 more times; an excellent stimulator of metabolic processes;
- honey massage: apply warm liquid honey to the ankles before going to bed and rub lightly, massaging the tissues for 5 minutes; then wrap your feet in a warm cloth and leave until morning; restores blood circulation and metabolism in cartilage tissue.
Approach to treatment in clinics
Clinicians at the clinic have developed their own approach to treating diseases such as ankle and foot arthrosis. During the initial appointment, a thorough examination of the patient is performed, the doctor carefully listens to his or her complaints and the history of the disease, and then prescribes further laboratory and instrumental examinations, including MRI. Only then does the doctor establish the final diagnosis, prescribe and agree with the patient on the complex treatment. It consists of:
- modern schemes of pharmacological and non-pharmacological treatment of arthrosis - drugs, physiotherapy, gymnastics and massage, ankle fixation methods;
- traditional methods of oriental therapy - acupuncture, moxibustion, acupressure, various kinesiotherapy methods, including taping.
This is not all the methods used in clinics. Physicians are able to combine Western and Eastern methods, significantly accelerating the improvement of the patient’s condition. Patients get rid of pain quickly and their quality of life improves significantly.
A combination of Eastern best practices and innovative methods of Western medicine.
Prevention of arthrosis of the foot
To reduce the risk of disease progression, the following recommendations should be followed:
- activity, exercise therapy exercises, swimming should become a part of your life;
- high levels of physical activity and traumatic factors should be ruled out; hiking should be combined with rest, if the legs are injured during work, it is worth replacing;
- injuries, especially on ice in winter, should be ruled out by considering the modes of movement and the shoes used;
- rational nutrition is needed to restore metabolism, but being overweight puts extra strain on your ankles, get rid of it;
- preventive treatment courses are a guarantee of a painless life.
Frequently asked questions about the disease
- Which doctor should I go to for ankle osteoarthritis and leg arthrosis?
To the orthopedic traumatologist. But if the disease developed in the background of some rheumatic process, then to a rheumatologist.
- What predictions do doctors usually give?
At any stage, the progress of the degenerative process can be stopped and the quality of life improved, but it is best to do so at the onset of the disease, not to wait for complications to appear.
- Can ankle arthrosis develop in children?
Maybe after an injury or a background of congenital pathology.
- What are the consequences of the disease?
Untreated arthrosis leads to disability. If you start treatment on time, your limb function can be very well preserved. Subsequent treatments relieve pain and improve quality of life.
- Causes of sports injuries for ankle osteoarthritis?
Yes, sports injuries are one of the main causes of this disease.
- Is it possible to do ankle banding for arthrosis?
It is possible, but this must be done by a professional.
Anthrax of the ankle joint is almost always the result of macro- or microtrauma. At first, it moves slowly and unnoticed. Therefore, timely treatment and rehabilitation after injuries, as well as seeing a doctor for the first signs of ankle disease, are very important.































